Many approaches to therapy are considered. The decision on the nature of the treatment depends on many factors. In summary, the therapy approaches are similar to those for natural teeth.
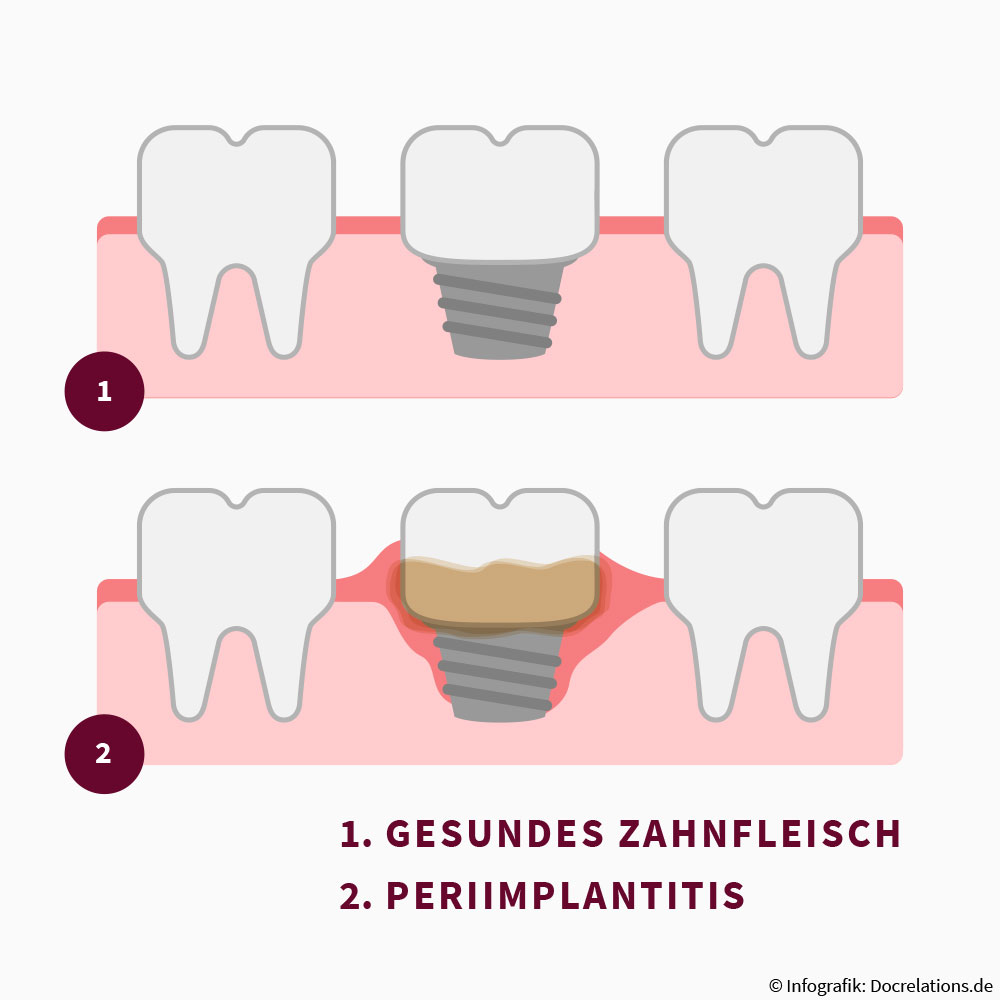
Peri-implantitis is a disease which may affect people who have dental implants. It generally develops as a result of defective oral hygiene and implant care. As a result of this, food residues, bacteria and the components of saliva may accumulate – as also occurs with natural teeth. What follows is similar to periodontitis of the natural tooth: inflammation develops, mucosa and bone may recede.
If the peri-implantitis is not treated, dental implant loss may occur. For therapy, we perform a professional cleaning of the implant. Furthermore, the patient must use anti-infectious and antimicrobial rinsing solutions for about four weeks.
Do you have any questions?
Or are you interested in our periodontitis procedures? Call us or write to us:
Frequently asked questions about peri-implantitis therapy
When the gum tissue that surrounds the implant – the new artificial tooth root – becomes inflamed, (peri-implant) mucositis is present.
If this condition is identified early and appropriately treated, the inflammation can be stopped. It generally heals completely, without leaving damage to the implant.
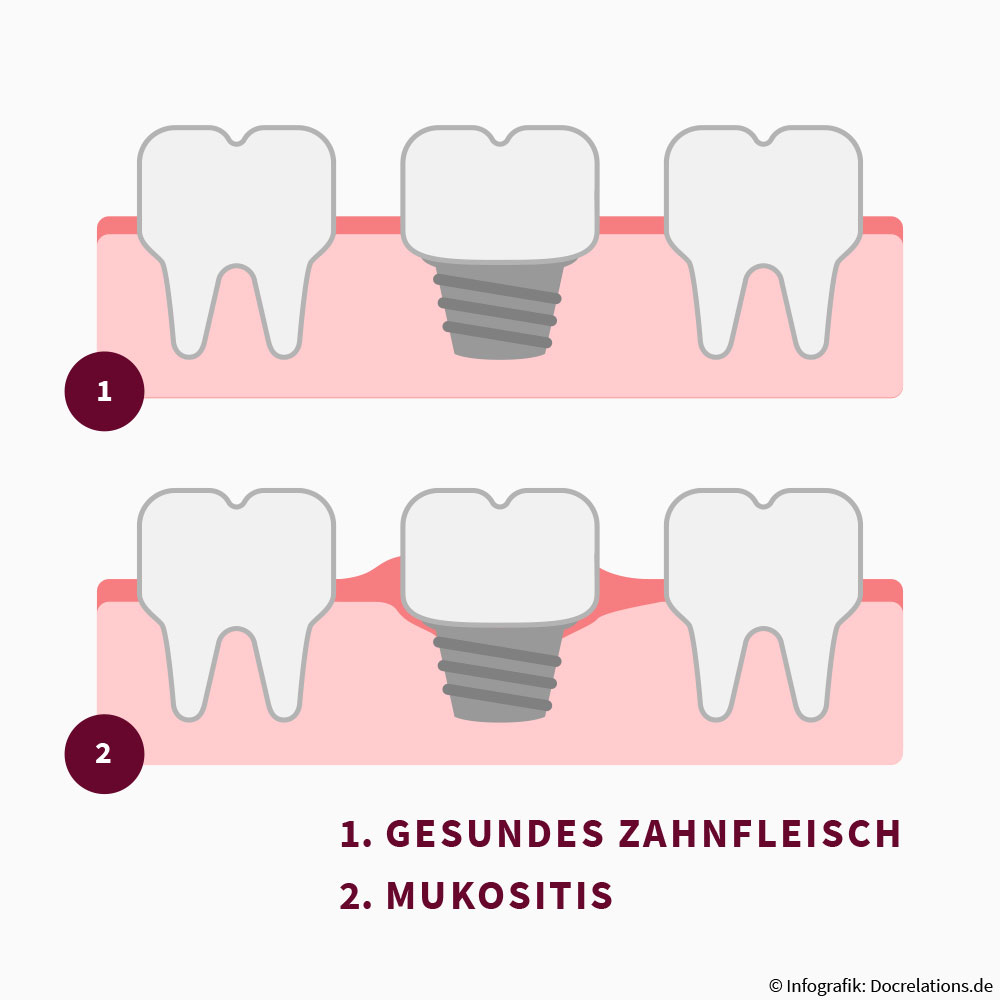
If the mucositis remains undetected or is not treated promptly, peri-implantitis may occur. Bacterial inflammation progresses so far here that it is not only the gum around the implant but also the jaw bone that is infected.
There is a risk that the bone recedes and the implant can no longer be retained. The replacement teeth may come loose and no longer fulfil their purpose.
In the worst case, implant loss occurs. Thus, a new kind of tooth replacement is needed so that the gap that develops can be closed.
General factors
In a similar way to gingivitis and inflammation of the periodontium (periodontitis), mucositis and peri-implantitis are the result of bacterial infection.
The cause of infection is often unsatisfactory dental hygiene or oral hygiene. If the patient’s dental plaque is not removed regularly and with sufficient thoroughness, bacteria can stick to it. The bacteria may advance from the gum margin to the neck of the tooth implant and lead to inflammatory reactions there.
Further reasons for inflammation after implantation are as follows: irregular dental assessments, untreated or inadequately treated periodontitis, a disorder in the implant healing phase, systemic diseases such as diabetes or osteoporosis, changes in hormone balance, side effects of certain medications, heavy smoking, stress or a generally elevated risk of developing inflammation.
Local factors
As well as the general factors mentioned above, what are known as local factors may lead to problems with the implant.
These include micromovements between the artificial tooth root and the abutment, i.e. the part connecting the implant to the new tooth crown. Leakage at the inner connection in the implant is also a possibility.
If inflammation occurs after implantation, this initially manifests as mild tenderness which generally occurs when the swollen gum in the vicinity of the implant is touched. The dentures themselves may cause pain.
Reddening of the gum margin in the affected places is also indicative of inflammation. In some cases, pus forms around the implant neck.
Later, pain may occur in the jaw bone. The gum in the vicinity of the implant often recedes. Many patients feel that the implant is loosening.
Sweet-smelling breath may be a further symptom of peri-implantitis.
We rapidly suspect peri-implantitis from the symptoms described by the patient.
To confirm the diagnosis – or to exclude other conditions –, there are different options available to us.
Marker test/aMMP-8 tests
We take a sample with a test strip in the vicinity of the implant and examine it for the aMMP-8 collagenase value. These are enzymes that degrade tissue substance. If the value is elevated, inflammation of the implant bed or peri-implantitis is present.
Examination with the periodontal probe
In this examination, we insert a periodontal probe into the gum pocket in the vicinity of the tooth implant. If pus or blood come out, this is a clear indication of inflammation of the implant bed.
X-ray
From X-ray examination with our highly modern and low-radiation 3D X-ray system (digital volume tomography DVT) we obtain an exact three-dimensional image of the jaw and can make an optimal assessment of the situation.
On the international level, about one third of all implant patients develop peri-implantitis.
Yes, peri-implantitis can occur with both titanium and ceramic implants.
The aim of therapy of implant bed inflammation is to eliminate the inflammation completely. The individual procedure depends on the stage of the disease and on the species of bacteria that predominate in the patients. In general, we treat peri-implantitis surgically. In some cases, it may be necessary to take antibiotics.
It is possible to restore the lost bone substance when the inflammation has completely healed. This requires another surgical procedure, in which the jaw bone is filled with bone substitute material. Then the bone has the potential to regenerate. Depending on the success of this treatment, the attempt to insert another implant can be started anew.
Don’t worry – all therapies in our practice that may cause pain are performed under local anaesthesia. With local anaesthesia, we can eliminate the sensation of pain in the region to be treated. You feel nothing. When the anaesthesia wears off and you feel mild pain, this can be treated with conventional analgesics.
The duration of peri-implantitis therapy depends on the severity of the disease. In addition, individual factors and any special anatomical features play a role. We draw up your personal treatment plan during the examination and the subsequent discussion of findings. This can be adapted to your time management.
The following generally applies: If the peri-implantitis is far advanced, explantation, that is the removal of the implant, may be necessary.
Whether and when explantation has to be performed is one of the most difficult questions in dental practice. In general, explantation should be considered when it is no longer worth preserving the implant for economic and/or aesthetic reasons. Nevertheless, an initial attempt to preserve the tooth should always be made – especially when the remaining bone anchorage permits this.
You’re in the best of hands with us!